The Profound Effect of Childhood Trauma; A Gentle Revolution of Trauma Informed Care
“We are all impacted by trauma. We are all paying the cost whether personal or societal. We help people heal when we promote connections to one another.” ~ Dr. Vicky Kelly
Nowadays we are witnesses of significant trauma and the consequences of trauma every time we connect with social or commercial media. We are drawn into graphic displays of individual and community experiences which include violence, abuse, bullying, natural disasters, death, war, terrorism and the effects of an opioid epidemic. And so, trauma has moved to the forefront of national consciousness.It is important to note that every one of us has experienced some kind of trauma in our own lives as well. Trauma seems to be everywhere. Of course, it is. And it always has been. But with our increased awareness of the pervasiveness of trauma and our collective brokenness, a gentle revolution has evolved. We have created and are developing behavioral, medical and mental health services that are effectively healing childhood and adult trauma. This new approach to what the CDC is calling perhaps the single biggest healthcare problem facing our nation today is called Trauma-Informed Care (TIC).Just what is Trauma-Informed Care?Trauma-Informed Care (TIC) is one of the most exciting things to happen in the way we provide psychosocial treatment (behavioral health) services for children and adults. We are shifting our perspective and treatment model from one which asks “What is the matter with you?” to “What happened to you…and how does that impact your life and functioning today?” This basic modification in approach is offering a dramatic new strategy which is helping people cope and heal. We are now equipped with new, extensive research and information about trauma, development, and the brain.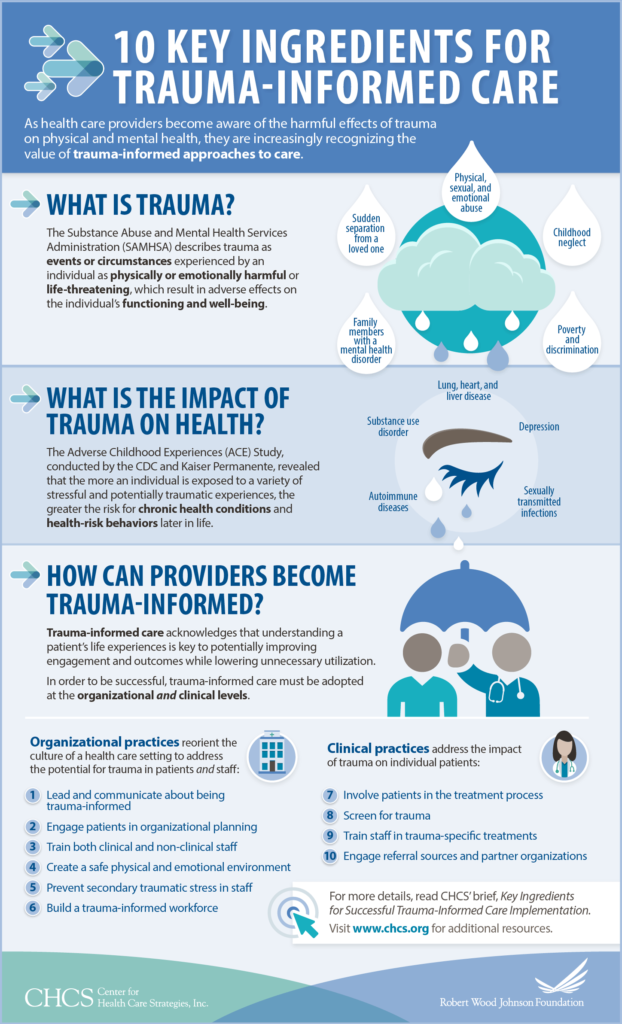 We begin to be trauma-informed when we understand what trauma is;“Individual trauma results from an event, series of events, or set of circumstances that is experienced by an individual as physically or emotionally harmful or life-threatening and that has lasting adverse effects on the individual’s functioning and mental, physical, social, emotional, or spiritual well-being.” ~ Substance Abuse and Mental Health Services Administration (SAMHSA)There you have it. SAMSHA gives us a good definition of trauma. With that understanding, you have just become more trauma-informed. And I believe that being trauma-informed is a way we can shape the future.Where Did the TIC Model Come From?The stage was set for Trauma-Informed Care by two major research studies.
We begin to be trauma-informed when we understand what trauma is;“Individual trauma results from an event, series of events, or set of circumstances that is experienced by an individual as physically or emotionally harmful or life-threatening and that has lasting adverse effects on the individual’s functioning and mental, physical, social, emotional, or spiritual well-being.” ~ Substance Abuse and Mental Health Services Administration (SAMHSA)There you have it. SAMSHA gives us a good definition of trauma. With that understanding, you have just become more trauma-informed. And I believe that being trauma-informed is a way we can shape the future.Where Did the TIC Model Come From?The stage was set for Trauma-Informed Care by two major research studies.
- Adverse Childhood Experiences (ACEs) Study (Kaiser Permanente from 1995 to 1997 and Centers for Disease Control and Prevention, 2013) was a large epidemiological study involving more than 17,000 individuals from the United States; it analyzed the long-term effects of childhood and adolescent traumatic experiences on adult health risks, mental health, healthcare costs, and life expectancy.
- The Women, Co-Occurring Disorders and Violence Study (Multiple studies from 1998 to SAMHSA, 2007) was a large multisite study focused on the role of interpersonal and other traumatic stressors among women; the interrelatedness of trauma, violence, and co-occurring substance use and mental disorders; and the incorporation of trauma-informed and trauma-specific principles, models, and services.
These two studies generated action within the behavioral health systems creating a basic adjustment from short term biomedical/pharmaceutical and behavior modification in nature (diagnosis and symptom treatment) to a longer-term, holistic model of neurological healing which treats the set of circumstances that have created the trauma/stress. We have not abandoned the other treatments altogether of course. There is still a place for medications and traditional methodology. We have just found a new and more effective approach.Trauma-Informed Care Comes From a Brain ThingWe can now help brains heal and rewire with Trauma-Informed Care. As a result, there is new hope for victims of adult PTSD and Developmental Trauma Disorder (Childhood PTSD). Studies show that a healthy well-regulated brain where the thinking brain and survival brain work well in tandem can be facilitated with TIC.It helps to understand that we have two brains and a mediator. The thinking brain is the Cortex. It is where our personality lives, where we make good decisions, and where our memories are stored. This is where we receive information, process it and take action based on that information. The other brain is the midbrain and brainstem also known as the survival brain. It is out autopilot. and runs our bodies so that we don’t have to think about those functions It is where we are told to breathe, where our heart is told to beat, and where we are informed about how to digest food. It is also where fight, flight and freeze responses reside. Trauma and stress have particular influence on the survival brain. The important mediator in the brain called the Thalamus which receives sensory information (sight, sound, touch, taste) and acts as a relay station that sends a signal to both brains. The survival brain is wired faster than thinking brain (because the faster you react the more likely you are to survive).Here is why this is so vital to trauma-informed care. The brains of adults who suffer from PTSD and children with Developmental Trauma Disorder have been hyper-activated or hyper-aroused. A soldier who is constantly facing an enemy who wants to kill him or a child who is being sexually, physically or emotionally abused is in a survival brain mode of operation of fight, flight or freeze twenty-four hours a day. When that soldier returns home from war, or when the abused child is placed in another home the brain is still programmed to expect trauma or abuse. The thinking brain has been informed of the change but the survival brain is still hyper-activated. They cannot think their way out of new stressful situations but react with programmed survival brain responses.Traumatized brain impacts:
- Fear and lack of safety in the adult or child’s environment cause automatic conditioned behavioral responses of fight, flight and freeze (along with more complicated survival responses such as hiding, withdrawing, pretending, and so on). Brain studies show that the survival brain literally hijacks (turns off) the thinking brain. In other words, the traumatized brain cannot effectively discern good decisions from bad decisions because it cannot always access the thinking brain.
- The brain’s alarm system for danger becomes distorted. The traumatized brain perceives the presence of danger almost everywhere. Impedes the ability to find help and establish relationships.
- An inability to appraise the present and to learn from experience. The traumatized brain becomes Velcro for bad and Teflon for good. Such that good experiences in later life cannot balance the negative trauma experiences of the past (childhood).
Now that we know all of these things about the brain and can actually see how it works in brain imaging and brain scans we are tasked with doing things to reduce the stress from trauma.The hurt happens in powerful childhood relationships and it takes new relationships to promote the healing. We have found that Trauma-Informed Care actually causes the brain to reprogram.TIC; A ‘Best Practice’ for Kids and AdultsDuring my 48 years as a provider of behavioral services for children and adolescents, I have seen the worst kinds of things that can happen to my clients. They have suffered multiple stressors that most people could never imagine. And the effects are cumulative. These are kids who have been physically and sexually abused. They have experienced their mothers enduring domestic violence and other disturbing chaos at home. Many witness chronic substance abuse and the effects of mental illness every day along with frequent incarceration of family members. They are dependent and neglected.Trauma-Informed care has allowed me to see my clients through a new pair of glasses. I believe that this exciting treatment model is the emerging framework for human service delivery. Until recently, the toxic stress and trauma these kids faced went largely untreated or undertreated. Trauma-Informed Care is now effectively healing the effects of the traumatic events which result in adverse physical, social, emotional, or spiritual consequences. One example of a TIC program in action can be found at St. Aemilian-Lakeside in Milwaukee, Wisconsin. SaintA is in the forefront of trauma-informed care therapeutic practices. They teach that there are seven essential ingredients in understanding what trauma-informed care is and how to implement it. These elements are;
- Prevalence — Exposure to and difficulty adjusting to adverse experiences is significantly more common than we previously had known. A keen appreciation for the scope of adverse events, especially on children, is a key element to understanding the needs of people who have been exposed to events such as domestic violence and substance abuse, separation/divorce, mental illness, physical and sexual abuse, emotional and physical neglect, and acts of violence.
- Impact — Trauma occurs when a person’s ability to cope with an adverse event is overwhelmed and contributes to difficulties in functioning. The impact of this process is profound, especially when the adverse event occurs during key developmental timeframes. The seminal ACE (adverse childhood experiences) study shows how early trauma also can have a serious effect on a person’s physical health in later life and ultimately impact life expectancy.
- Perspective Shift — A shift in perspective can bring a new reality. Helping those charged with caring for people struggling with trauma by simply changing the question from “What is wrong with you?” to “What has happened to you and how can I support you?” can bring enormous understanding.
- Regulation — Knowledge of the basic architecture of the brain provides both an understanding of the impact of trauma and a key toward effective treatment. Many of the interventions that have been offered to people struggling with trauma have focused on the cognitive or “thinking” parts of the brain. Trauma-informed interventions often prioritize enhancing emotional and behavioral regulation. This could include the use of sensory and regulating strategies such as drumming, singing, dancing, yoga, etc., which have been shown to be effective in addressing the impact of trauma.
- Relationship — Relationships are key to reaching a traumatized child and to mitigating trauma. Strong relationships help create resilience and shield a child from the effects of trauma.
- Reason to Be — Reason to be creates a sense of purpose or direction for individuals by ensuring they’re connected to family, community, and culture. It is bolstered by resiliency – a combination of the individual’s internal attributes and the external resources that support them.
- Caregiver Capacity — To effectively work with traumatized individuals, caregivers must take care of themselves and find a work/life balance. Critical is identifying our limits, knowing sometimes we will be pushed beyond them, and what we will do to find balance.
They have a YouTube video which is terrific at telling the story of Trauma Informed Care. I suggest that you connect with it at the following web address: https://www.youtube.com/watch?v=p_dZAqP_tfYSAMHSA offers some sobering statistics in their recent Treatment Improvement Protocol (TIP 57) that have compelled service providers of all stripes from educators to chaplains to behavior and mental health professionals to juvenile justice institutions and police officers to embrace trauma-specific interventions in their work. How can we not when we learn that;
- 71 percent of all children are exposed to violence every year
- 3 million children are maltreated or neglected each year
- 5-10 million kids witness violence against their mother each year
- 1 in 4 girls and 1 in 6 boys are sexually abused before adulthood
- 94 percent of children in juvenile justice settings have experienced extreme trauma
Finally, Trauma-Informed Care is about healing through building safe relationships and developing trust. When mentors extend a helping hand to kids and adults who have suffered so much they begin to develop a reason for being. Peer support and mutual self-help are also key vehicles for establishing safety and hope, building trust, enhancing collaboration, serving as models of recovery, healing, and maximizing a sense of empowerment.We can make this happen by encouraging politicians to sponsor ACEs and TIC legislation. We can make this happen by making noise in the public square at PTA meetings, Service Clubs, Town Hall gatherings and the like. We can make this happen by offering ourselves as available mentors. There is a groundswell of hope. 38 states and the District of Columbia are gearing up. It’s time to join the movement.Robert Kenneth Jones is an innovator in the treatment of addiction and childhood abuse.In a career spanning over four decades, his work helping people recover from childhood abuse and addiction has earned him the respect of his peers.His blog, An Elephant for Breakfast, testifies to the power of the human spirit to overcome the worst of life’s difficulties. We encourage you to visit and share this rich source of healing, inspiration and meditation.Contact Bob Jones on LinkedinBob Jones’ blog An Elephant for Breakfast